by Jennifer Cameron, Ph.D.
Tips for Improving Communication With Your Healthcare Providers
Let’s face it. No one’s favorite place to be is the doctor’s office. Yet we will all need medical care at some point, and effective communication will likely improve our experience. We may have many different emotions going into any given visit, and we may also have things that we want the healthcare clinician to understand about us. Sometimes we have questions that we want answered. Our feelings, message and questions may even change as a visit progresses. Since we know from research that the quality of communication with a healthcare team is important, there are some ways to help us keep track and get the most out of our healthcare appointments. Below are some considerations for communicating with your clinicians.

One of the most powerful tool sets you can use is a pen and paper, or notes on your phone. Checking in with yourself about your priorities for the appointment and writing them down before the visit can provide direction for your healthcare. Some priorities and possible language you may use include:
- To be understood: “The three most important things for me on this visit are…” Succinctly stating upfront what you most want to communicate to the clinician can guide your time together. It lets the clinician know exactly what you want them to know about your experience.
- To gain education: “I want to understand what is happening with my body.” Your focus may be on understanding a symptom or medical condition, rather than jump straight to a test, medication or treatment. Stating this preference offers the clinician an opportunity to meet you where you are.
- To receive decisional support: “I want guidance about treatment options, and assistance weighing the risks and benefits of those options.” Learning about your options – and the pros and woes of those options – can be an overwhelming experience. Asking your clinician to help you understand the risk and benefits communicates what you most need from them at the moment.
- To clarify: “What are my options if this initial treatment doesn’t turn out as hoped?” “How do I reach you or someone covering for you if I have a flare outside of regular business hours?” Having information about potential next steps in your care can help you to take charge of your healthcare. If a condition is likely to change suddenly, working together on a plan of care empowers you to know the first steps to take when a flare up occurs.
Back to that pen and paper – take notes during the visit. Writing down key words and recommendations from the clinician, and any additional thoughts that may come up for you as your conversation develops, can help you to more fully take in what the clinician is saying and touch base with what you are thinking and feeling.
It can also help you to ask the clinician if you can summarize to them what you understand about your visit. Using this teach-back method gives you an opportunity for ensuring that you and the clinician have a shared understanding of your time together. Although you may have a good grasp based on your conversation, repeating it aloud confirms that you do and offers a great opportunity for follow-up questions. Writing down the outcomes of the visit, or asking the clinician for their written or printed recommendations and plan, helps to recall those tidbits that may be easily forgoten.
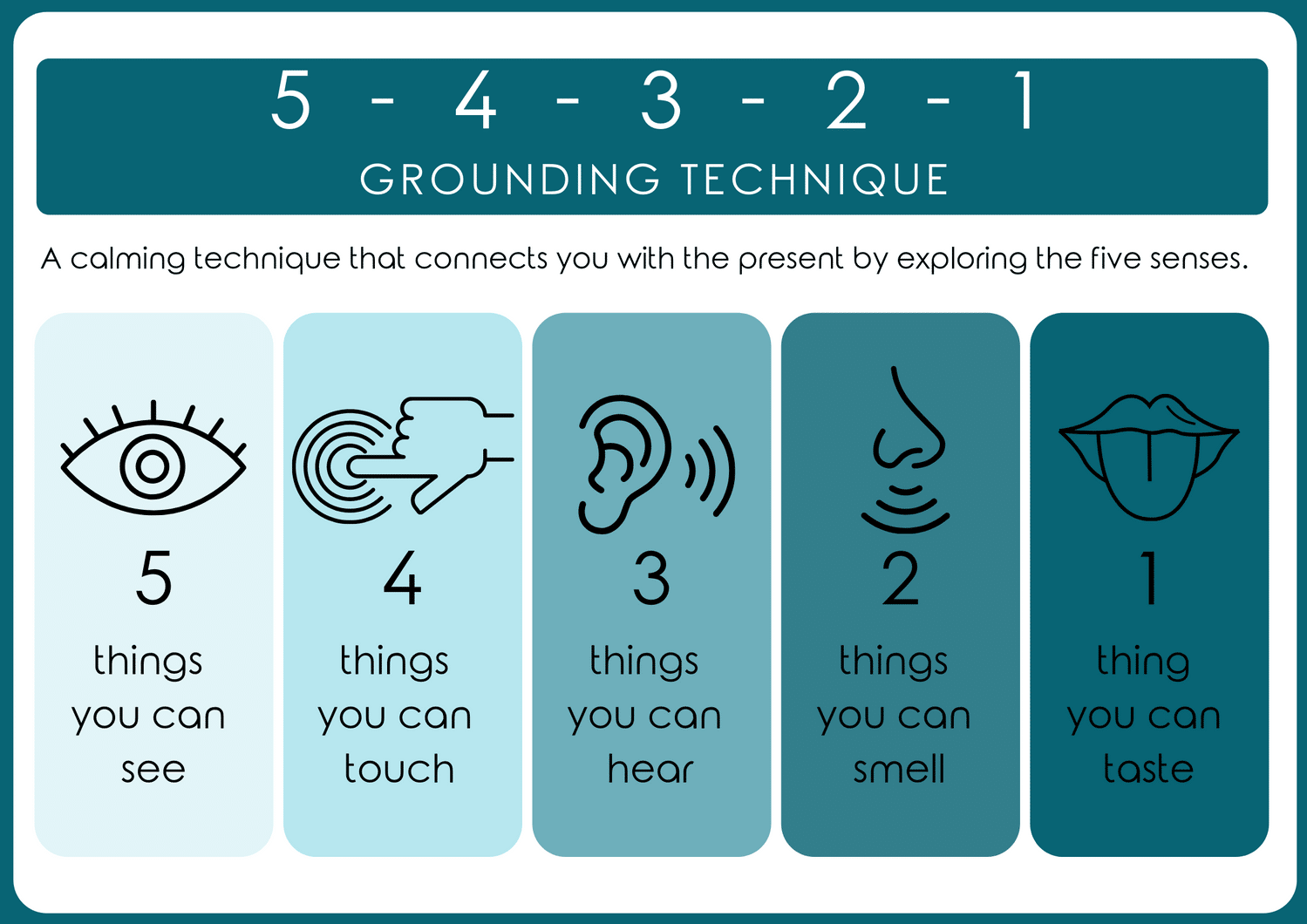
One more tool. Most medical offices will have an opportunity for you to pause between contacts with the members of your medical team. Those moments can be an opportunity to practice mindful breathing, try grounding strategies, or listen to a calming sound such as the ocean while you wait. Staying grounded and mindful in this way can help to keep you focused on your priorities, especially in the context of what can be a busy and sometimes anxiety-provoking setting.
Bottomline – we all have an underlying need to be understood, especially when it comes to our health. Being prepared before and engaging during a visit offers the clinician a better chance of meeting us where we are. Although any interaction between two humans is rarely perfect, these strategies can help us build a stronger foundation for managing our healthcare visits.
Jennifer Cameron, Ph.D. is a medical psychologist licensed in North Carolina and Virginia. She is passionate about providing care for individuals experiencing difficulties that occur at the intersection of mental and physical health. Her experience and training as a specialist in the fields of Behavioral Medicine and Behavioral Health Integration uniquely position her to serve clients seeking support for emotional distress related to physical or medical issues. She excels in helping clients create effective health plans and engage in behaviors that help them move towards meaningful change. If you are interested in learning more about how working with Dr. Cameron can improve your mental and physical wellbeing, you can read her bio. To schedule an appointment with or refer to Dr. Cameron, please use our contact form or reach out to our front desk at [email protected].





